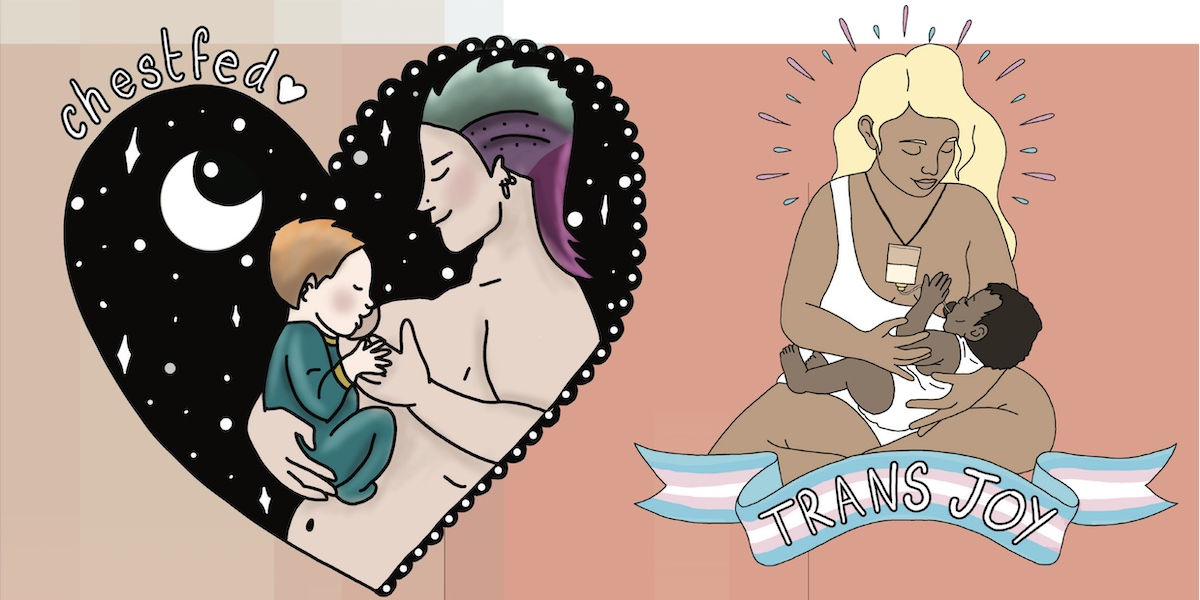
AJ Silver on queer birthing
‘LGBTQ+ people are not the expected service users in the maternity and perinatal sector. Pathways to funding, forms, computer systems, referral criteria, language and the education of health care professionals and birth workers have all been designed with cisgender/heterosexual people in mind. When LGBTQ+ families navigate these systems, we often fall through the cracks.
Many health care professionals and birth workers were educated during the Section 28 legislation, which made illegal the ‘promotion of homosexuality as a pretended family relationship’ during 1988-2003. Lack of education is one of the underlying issues behind the challenges LGBTQ+ people face. The lack of individualised language and terminology can further inequalities.
Trans and non-binary people experience huge disparities in healthcare access and outcomes. In the UK society, hate crimes against trans and non-binary people have increased dramatically. Health care professionals need to ensure they are doing all they can to ensure trans and non-binary pregnant people have suitable access to individualised and humanising care.
The Queer Birth Club offers LGBTQ+ competency workshops for birth workers and healthcare professionals, explaining language and terminology and statistics as well as LGBTQ+ history and case studies, allyship and more. Ask your NHS trust or educational setting to provide LGBTQ+ materials.https://uk.jkp.com/products/supporting-queer-birth
Excellent free insights into LGBTQ+ experiences include Seahorse, The Dad who Gave Birth (BBC iPlayer), Our Baby: A Modern Miracle (Channel 4) and the podcasts Pride & Joy and Pride In Birth. There is also a growing base of research on LGBTQ+ conception, birth and the perinatal period, including journal articles at aims.org.uk.‘
Molly O’Brien on outdated medical models
‘Medical language subjugates women. In textbooks and hospitals around the UK, when a woman faces difficulties in labour she might hear ‘failure to progress’. Or the more derogatory ‘inefficient contractions’, ‘inadequate pelvis’, even ‘insufficient maternal effort’.
Instead of the symptoms, we should examine the root causes of difficulties during birth. I teach that these are linked to biomechanics. We must listen to what women say about their bodies. Health professionals treat them as if their body is not very well made or tell women they’re risking their babies’ lives if they don’t listen to medical advice.
In the UK, we are still working on the 1938 Caldwell and Moloy model on pelvic types. It defines the ‘normal’ type and mechanisms of how the baby passes through the pelvis. The model is racist. It’s based on a European study. What about women from other parts of the world?
Studies show that pelvic shapes exist on a spectrum. Relying on an outdated model influences clinical behaviour, placing judgement on women, especially black women, and encourages unnecessary medical interventions – induction, C-sections, use of forceps – which impact the woman’s and baby’s body post-birth.
People end up carrying trauma with them, maybe for the rest of their lives. Some physical harm is life changing. Pelvic prolapse, for instance, is common. Instead of support, we have advertisers selling lacy pants so we can ‘feel sexy’ while suffering incontinence as a result of a birth. Women deserve more.‘
Devon Price on hormone damage
‘A battle is playing out in UK courts, parliament and the NHS over whether transgender teens can meaningfully consent to taking puberty blockers. The argument behind this curtailing of trans people’s rights is that the medications’ effects are not sufficiently known and may have permanent effects that later become unwanted.
I am a transgender person. I felt pressured into taking hormones with poorly studied and at-times irreversible effects. It was the birth control I was put on at 18, not the hormone replacement therapy (HRT) I take now.
My friends were pushed onto the pill by anxious parents, by boyfriends, by doctors saying it would manage painful and irregular periods, or just to get rid of body hair or spots. It had significant effects on my body, some permanent, hyper-feminising it in ways I hated: my breasts ballooned, my body became softer, my face rounder, my body hair lighter.
I was despairing a week before my period, every single month. People have reported negative mood effects from hormonal birth control since the 1970s. Research attesting to that only found traction in the 2010s. To this day many medical professionals deny links between contraceptives, depression and suicide, despite the evidence.
The pill has also changed countless lives for the better. I would never advocate for restricting access to it. The problem isn’t its existence or accessibility. I took it because I lived in a sexist, coercive society that hadn’t listened to the people clamouring for better options, for decades. We still need better research and to listen to users. The informed consent model that works well for trans people accessing hormones, like me, could offer a blueprint for respectful engagement with teens looking into contraceptives.
We also need more research into providing quality healthcare to trans people. Doctors generally don’t care about our experiences or our long- term health outcomes. They get away with mistreating trans patients, particularly trans women, because we are so roundly dehumanised. Restricting access to HRT and hormone blockers – denying our agency – won’t fix that. Studying the risks that come with all hormonal medical treatments and informing people about them – rather than fear- mongering – can empower us all to make healthy choices about our own bodies.‘
– This is an extract from aninjusticemag.com
UK fact file on pregnancy, birthing and labour
- Twenty-six per cent of women aged 16-49 years use hormonal contraception
- Maternal mortality in the UK has risen by nearly 20 per cent in recent years, with suicide now the main cause of death. Women living in the most deprived areas are twice as likely to die in pregnancy and childbirth as those in the most affluent parts of the UK. Black women are four times more likely to die, and Asian and mixed-race women twice as likely as white women
- A 2022 Care Quality Commission’s report highlights England’s maternity services as an ‘area of special concern’. Two in five maternity service units are ‘not good enough’
- The UK ranks ninth lowest of 33 European countries for ‘full-rate equivalent‘ paid maternity leave
- Due to poor IVF funding, NHS England and Wales trusts often cannot offer the recommended cycles per person. Some refuse to treat women over 35, those who cannot prove they are in a ‘stable relationship’, or couples where one partner has a child from a previous relationship. Same-sex female couples in some areas must first prove infertility by self-funding 12 rounds of artificial insemination, which costs approximately £26,000